Download Free Epc Dental Programs Medicare
- Download Free Epc Dental Programs Medicare Advantage
- Download Free Epc Dental Programs Medicare Plans
- Download Free Epc Dental Programs Medicare Supplement
- Medicare Epcs Requirements
- Epcs Medicare Part D
- Download Free Epc Dental Programs Medicare Insurance
Chronic Disease Management - Individual Allied Health Services under Medicare - Provider Information (PDF 374 KB)
If you have any difficulty accessing the PDF, please email the Medical Benefits Division Webmaster.
People with chronic conditions and complex care needs – items 10950 to 10970
This fact sheet must be read in conjunction with the item descriptors and explanatory notes for items 10950 to 10970 (as set out in the Medicare Benefits Schedule - Allied Health Services book).Summary:
Use the menu below to select and download data used in Medicare drug and health plans, including Medigap, Medicare Plan Finder, Medicare Prescription Drug Plans and Medicare Advantage Plans. Downloadable databases are available as zipped Microsoft Access databases and also in CSV (comma separated values) format for some databases. The CDPHP Enhanced Primary Care Program (EPC) is an innovative patient-centered medical home (PCMH) model that offers financial rewards for providers and helps members live their healthiest lives. The EPC program.
- A Medicare rebate is available for a maximum of five services per patient each calendar year. Additional services are not possible in any circumstances.
- If a provider accepts the Medicare benefit as full payment for the service, there will be no out-of-pocket cost. If not, the patient will have to pay the difference between the fee charged and the Medicare rebate.
- Patients must have a GP Management Plan and Team Care Arrangements prepared by their GP, or be residents of a residential aged care facility who are managed under a multidisciplinary care plan.
- Referrals to allied health providers must be from GPs.
- Allied health providers must report back to the referring GP.
Eligible Patients
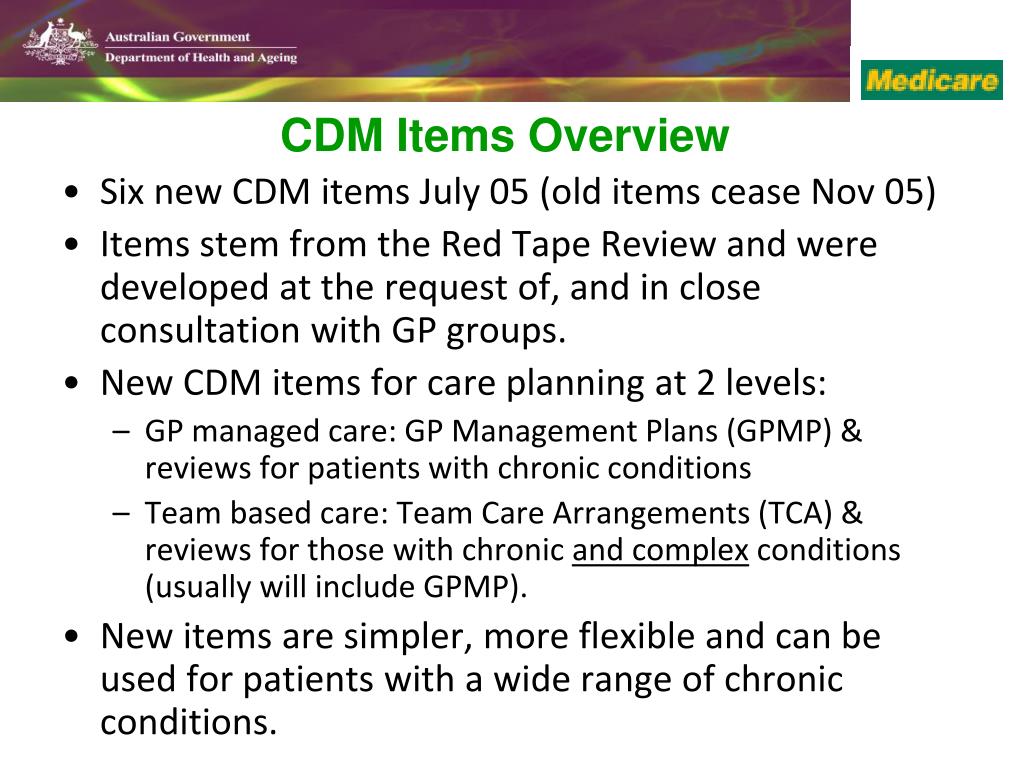 Community-based patients may be eligible if they have a chronic (or terminal) medical condition and their GP has provided the following Chronic Disease Management (CDM) services:
Community-based patients may be eligible if they have a chronic (or terminal) medical condition and their GP has provided the following Chronic Disease Management (CDM) services: - A GP Management Plan (GPMP) - (item 721) and
- Team Care Arrangements (TCAs) - (item 723).
A chronic medical condition is one that has been (or is likely to be) present for six months or longer, for example, asthma, cancer, cardiovascular disease, diabetes, musculoskeletal conditions and stroke. There is no list of eligible conditions. However, the CDM items are designed for patients who require a structured approach and to enable GPs to plan and coordinate the care of patients with complex conditions requiring ongoing care from a multidisciplinary team.
Patients have complex care needs if they need ongoing care from a multidisciplinary team consisting of their GP and at least two other health or care providers.
Referral arrangements
The need for allied health services must be directly related to a patient’s chronic condition and identified in their care plan. GPs determine whether the patient’s chronic medical condition would benefit from allied health services.Patients need to be referred by their GP for services recommended in their care plan, using the referral form issued by the Department that can be found at the Department of Health website or a form that contains all the components of the Department’s form.
It is not appropriate for allied health providers to provide part-completed referral forms to GPs for signature, or to pre-empt the GP's decision about the services required by the patient.
Referral validity
A referral is valid for the stated number of services. If all services are not used during the calendar year in which the patient was referred, the unused services can be used in the next calendar year.However, those services will be counted towards the five rebates for allied health services available to the patient during that calendar year.
When all referred services have been used, or a referral to a different allied health provider is required, patients need to obtain a new referral.
Note: It is not necessary to have a new GPMP or TCAs prepared each calendar year in order to access a new referral(s) for eligible allied health services. Patients continue to be eligible for rebates for allied health services while they are being managed under a GPMP and TCAs as long as the need for eligible services continues to be recommended in their plan.Top of page
Service length and type
Services must be of at least 20 minutes duration and be provided to an individual patient. The allied health provider must personally attend the patient.Eligible allied health providers
Aboriginal Health Workers or Aboriginal and Torres Strait Islander Health Practitioners - item 10950Audiologists - item 10952
Chiropractors - item 10964
Diabetes Educators - item 10951
Dietitians- item 10954
Exercise Physiologists - item 10953
 Mental Health Workers* - item 10956
Mental Health Workers* - item 10956Occupational Therapists - item 10958
Osteopaths - item 10966
Physiotherapists
Download Free Epc Dental Programs Medicare Advantage
- item 10960Podiatrists - Item 10962
Psychologists - item 10968
Download Free Epc Dental Programs Medicare Plans
Speech Pathologists - item 10970
Download Free Epc Dental Programs Medicare Supplement
*includes Aboriginal health workers or Aboriginal and Torres Strait Islander Health Practitioners, mental health nurses, occupational therapists, psychologists and some social workers.
Allied health providers need to meet specific eligibility requirements, be in private practice and register with Medicare Australia. Registration forms are available from the Department of Human Services (Medicare) or can be obtained by phoning 132 150.
Allied health services funded by other Commonwealth or State programs are not eligible for Medicare rebates, except where a subsection 19(2) exemption has been granted.
Medicare Epcs Requirements
Reporting requirements - allied health providers to GP
 A written report is required after the first and last service, or more often if clinically necessary.
A written report is required after the first and last service, or more often if clinically necessary.Written reports should include any investigations, tests, and/or assessments carried out on the patient, any treatment provided and future management of the patient’s condition or problem.
More Information
Epcs Medicare Part D
The explanatory notes and item descriptors for these items are in the Medicare Benefits Schedule (MBS).For inquiries about eligibility, claiming, fees and rebates, call the Department of Human Services (Medicare): patient inquiries 132 011; provider inquiries 132 150.
Download Free Epc Dental Programs Medicare Insurance
In this section
